The Mental Health Act Video: Being Certified
Video Index
More Information
The BC Youth Mental Health Act video is a resource for youth (and their families) who need to stay in hospital to get treatment for a mental health issue.
This interactive video resource page is a quick but thorough guide to rights, options and opportunities, as well as links to further resources.

The BC Youth Mental Health Act video is a resource for youth (and their families) who need to stay in hospital to get treatment for a mental health issue.
This interactive video resource page is a quick but thorough guide to rights, options and opportunities, as well as links to further resources.

1.You have a serious mental health disorder that keeps you from dealing with situations or people around you safely.
2. You need medical treatment for the mental health disorder.
3. You need help in a hospital setting to stop the mental health disorder from getting worse or to stop you from hurting yourself or others.
4. You do not ask for this help voluntarily. And, you can’t be admitted voluntarily in case you refuse treatment or try to leave.

1. Guide to the Mental Health Act (2005)
https://www.health.gov.bc.ca/library/publications/year/2005/MentalHealthGuide.pdf
2. Mental Health Act

3. Access Pro Bono
1-877-762-6664 or 604-878-7400
Provides free legal information. Call them to get a 30 minute appointment for free.
4. Mental Health Law Program of the Community Legal Assistance Society (CLAS)
Provides advocates to represent patients at review panel hearings throughout the Province.
(604) 685-3425 or toll free at 1 888 685-6222
5. Legal aid societies
Patients may contact the local offices of the Legal Services Society which are listed in the local telephone directories or through
https://lss.bc.ca/legal_aid/legalAidLocations.php
6. Mental Health Review Board
https://www.bcmhrb.ca/i-am-a-patient/
7. BC Mental Health Rights
https://www.bcmentalhealthrights.ca/
Website by researchers at Simon Fraser University to help adults in BC better understand their Mental Health Act rights. On it you can find
-a pamphlet,
-a video,
-a wallet card, and
-posters
with rights information. The pamphlet, wallet card, and video captions are available in 9 languages. The site also features blog posts about mental health rights issues.
1. Certified
The Mental Health Act is a BC law that gives the reasons a person can be kept in the hospital against their will for mental health treatment of a mental disorder. This is called being “certified under the Mental Health Act.”
2. Criteria for certification
1) You have a serious mental health disorder that keeps you from dealing with situations or people around you safely;
2) You need medical treatment for the mental health disorder.
3) You need help in a hospital setting to stop the mental health disorder from getting worse or to stop you from hurting yourself or others;
4) You do not ask for this help voluntarily. And, you can’t be admitted voluntarily in case you refuse treatment or try to leave.
3. Doctor
Only a doctor (physician) licensed to practise medicine in British Columbia may certify a person under the Mental Health Act. The doctor does not have to be a psychiatrist.
4. Mental disorder
This term has specific legal meaning under the Mental Health Act. “Mental Disorder” is specifically defined in Section 1 of the Act as:
a disorder of the mind that requires treatment and seriously impairs the person’s ability
(a)to react appropriately to the person’s environment, or
(b)to associate with others.
5. Mental Health Review Board
An organization that coordinates Review Panel Hearings.
6. Mental Health Review Panel
For the purposes of a Review Panel Hearing, a review panel consists of the following persons:
a) a lawyer,
b) a doctor (a different doctor than the one on your treatment team), and
c) someone from the community.
7. Mental Health Review Panel Hearing
The Mental Health Review Board conducts hearings to review and decide whether persons certified should continue to be certified based on criteria in the act. People who are involved and present at the hearing include:
-the person (you) who is certified,
-the panel (see point #6 above),
-your treating doctor who is on your treatment team,
-and a lawyer or legal advocate.
A lawyer can give you legal information and advice, and help guide you through this process. Family may also be present.
https://www.bcmhrb.ca/i-am-a-patient/
8. Rights Under the Mental Health Act
You have the right:
• to know where you are, including the name and address of the hospital;
• to know why you have to stay;
• to speak to a lawyer. A lawyer is a person who can give you legal advice about your rights as a certified patient;
• to speak with a doctor regularly to check if you still meet the criteria for certification;
• to ask for another doctor’s opinion about your treatment.
• And, to ask for what is called a review panel hearing if you don’t agree with the doctor’s decision to certify you.
9. Treatment
Medical treatment related to the mental health issue, and includes medical tests such as bloodwork. Other examples include:
• talking one on one with staff or in a group
•working on challenges with your parents or other people in your life
• taking medication
• and practising what you are learning

Here are some activities suggested by other young people while staying at the hospital.
-Reading
-Art
-Watching a show/movie
-Playing guitar
-Crafts
-Yoga
-Deep breathing
-Talking to someone you trust
-Journaling
-Knitting
-Painting nails
-Drinking tea
The SELF Toolkit has lots of great ideas too:
https://keltymentalhealth.ca/sites/default/files/resources/SELF%20Toolkit%20Adolescent.pdf
Here are some of the forms that may be of interest and of use to you:
https://www2.gov.bc.ca/assets/gov/health/forms/3507.pdf
Schizophrenia:
Many SGAs are indicated as a first line therapy for schizophrenia in adolescents and for the positive symptoms of psychotic disorders in general. SGAs treat active psychosis as well as decrease relapses if remission from active symptoms is achieved.
Depression:
SGAs are not indicated for treatment of depression in adolescents unless a psychotic depression was present. For a depression without psychotic symptoms, first line treatment is an SSRI antidepressant. The potential side effects of SGAs and lack of clinical evidence supporting efficacy of SGAs in depression in adolescents without psychotic symptoms are both reasons SGAs would not be prescribed for this condition.
Bipolar Disorder:
Some SGAs are indicated for treatment of bipolar disorder in adolescents. They stabilize mood as well as treat psychotic symptoms associated with mania. SGAs can be used alone or in combination with mood stabilizers to treat bipolar disorder. Often they are used in combination with mood stabilizers especially to stabilize mania in its initial phase as the mood stabilizers are titrated up.
ADHD:
SGAs are not indicated to treat ADHD. They are sometimes used in conjunction with expert consultation for off-label, preferably third-line use, for short-term treatment for significant irritability and explosive emotions/behaviours while stabilizing on first-line and/or second-line treatment. First-line treatment for ADHD includes monotherapy with long acting stimulants; second-line treatment includes short-acting stimulants, atomoxetine, or guanfacine XR (alone or in combination with long-acting stimulants). Third-line treatments include clonidine (monotherapy or in combination with stimulants), bupropion or noradrenergic tricyclic antidepressants. Comorbidities should be treated with first-line treatments specific to the individual condition.
Eating Disorders (AN, BN, ARFID):
SGAs are primarily prescribed for symptom management in severe eating disorders in children and adolescents. There are mixed results for enduring effects on weight restoration and any potential benefits are balanced with the well-established risks. For treatment of AN, there are limited positive open-label studies with the use of olanzapine. Quetiapine and aripiprazole have even fewer studies with mild benefit noted at times. Risperidone does not have evidence for use in AN. Olanzapine has limited positive reports for use in ARFID. Use of SSRIs, specifically fluoxetine, has the most evidence for bulimia nervosa, in which high doses are demonstrated to reduce purging behaviour. There are risks for increased binging with SGAs in BN. SGAs are sometimes used off-label to help with emotional and behavioral regulation or depression and anxiety symptoms, but experts should be consulted prior to initiating treatment. Comorbidities should be treated with first line agents (NOTE: bupropion is contraindicated in eating disorders secondary to increased seizure risk).
1. Weight gain management guidelines:
Normal weight gain associated with growth and development
Recommendation: Repeat weight measurement at next scheduled screen. Provide information on the importance of lifestyle for decreasing risk of weight gain.
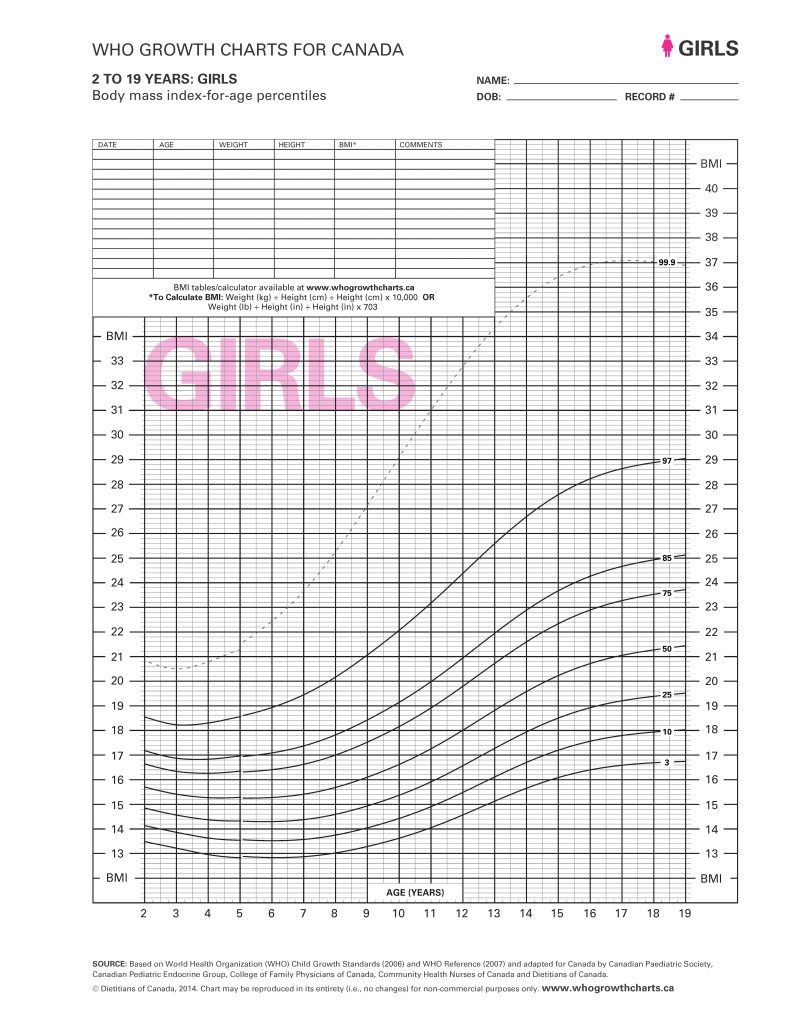
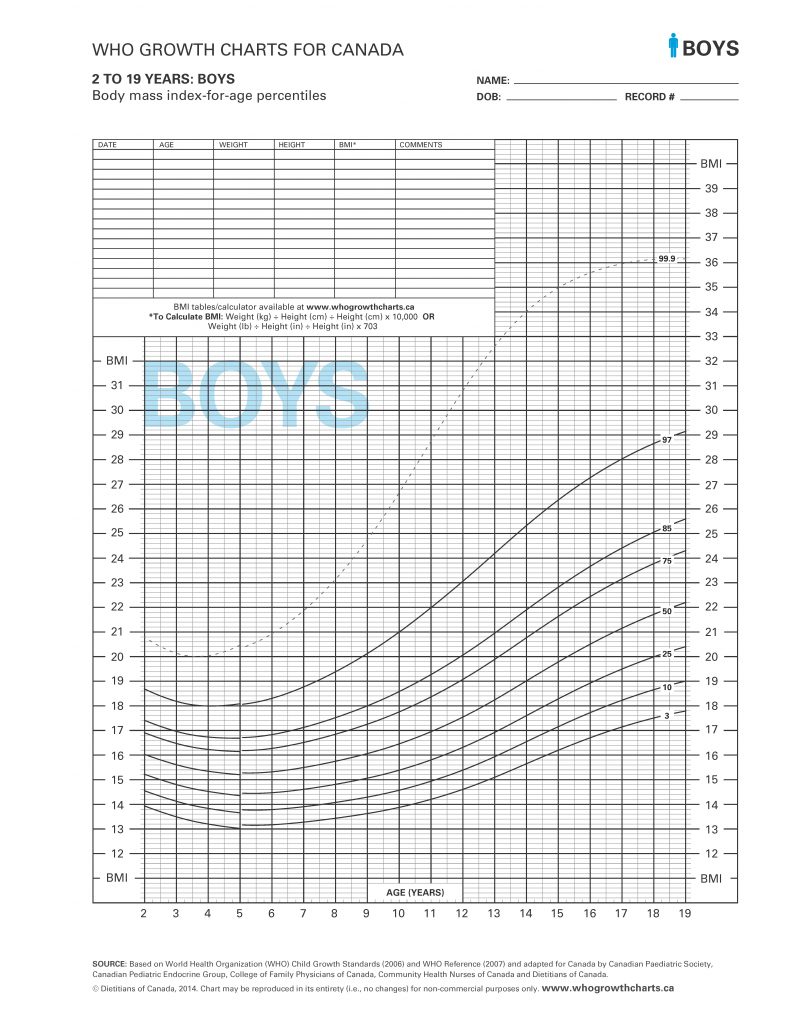
Significant weight gain noted, especially within first three months of medication use and/or child is overweight, obese or has pre-existing metabolic conditions prior to starting SGA treatment
Recommendation:
1.Lifestyle intervention
Second generation antipsychotic medication use in children and youth is associated with weight gain and metabolic complications. It is therefore strongly recommended that patients receive counselling (nutrition, lifestyle and exercise) at the initiation of therapy regardless of baseline body mass index. This is particularly important in a child who is overweight, obese or has existing metabolic symptoms prior to treatment with a second generation antipsychotic medication.
2. Re-evaluate use of SGA to minimize weight gain
Consider the following questions:
1. Abnormal prolactin management guidelines:
Elevations in prolactin levels may be associated with signs and symptoms such as gynecomastia, galactorrhea, infertility, menstrual irregularities, oligomenorrhea, amenorrhea, sexual dysfunction, decreased libido, acne and hirsutism in females. However, hyperprolactinemia may be asymptomatic in some individuals, particularly in prepubertal children.
Normal Prolactin
Recommendation: Repeat prolactin measurement at next scheduled screen.
Abnormal Prolactin
Recommendation: Re-evaluate use of SGA:
If continued treatment with the current SGA is essential for the patient’s psychiatric illness, consult with a specialist regarding further management of the hyperprolactinemia. There are potential long-term effects of hyperprolactinemia, particularly osteoporosis, even in asymptomatic patients. This is concerning given the importance of bone mineral accrual through adolescence with peak bone mass occurring in late adolescence.
If there are clinical concerns, consider specialist consultation for further investigation regarding other causes of hyperprolactinemia and/or amenorrhea.
2. Abnormal lipid fasting profile – triglycerides management guidelines:
B. Fasting lipid profile — Triglycerides
Normal TG < 1.5 mmol/L
Recommendation: Repeat TG measurement at next scheduled screen.
Normal TG ≥ 1.5 mmol/L
Recommendation: Re-evaluate use of SGA to minimize weight. Consider cognitive/behavioural lifestyle intervention aimed at weight loss. Consider consultation with specialist if TG ≥ 5 mmol/L for possible medical therapy.
1. Weight gain management guidelines:
Normal weight gain associated with growth and development
Recommendation: Repeat weight measurement at next scheduled screen. Provide information on the importance of lifestyle for decreasing risk of weight gain.
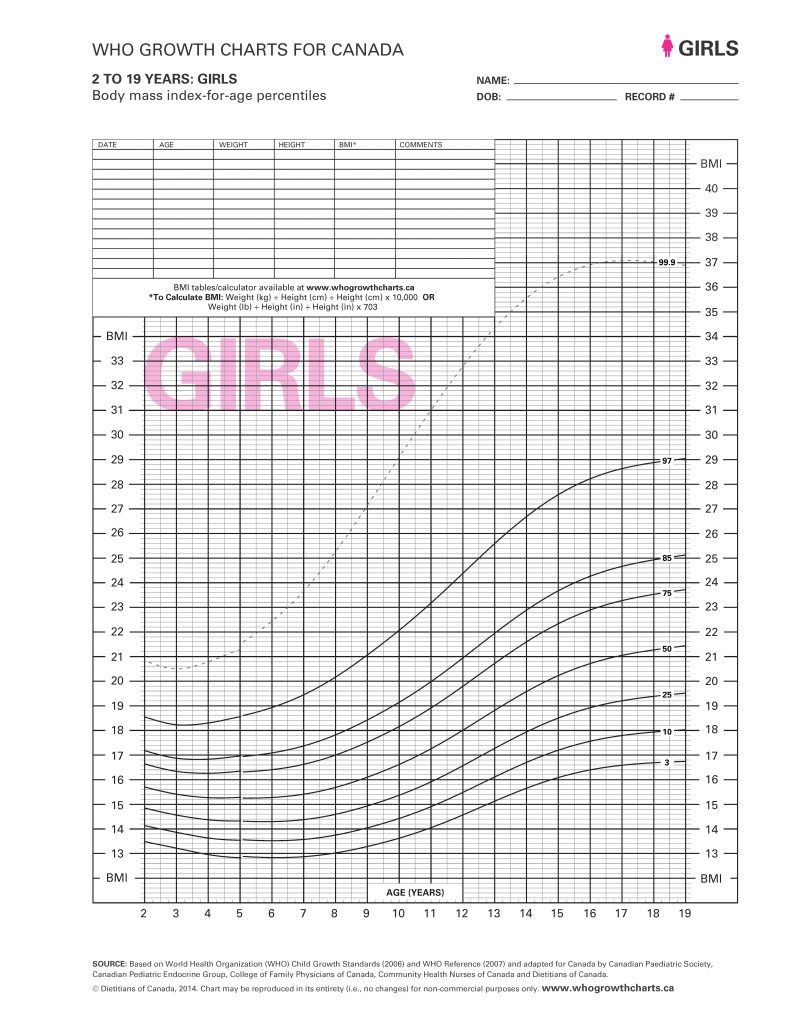
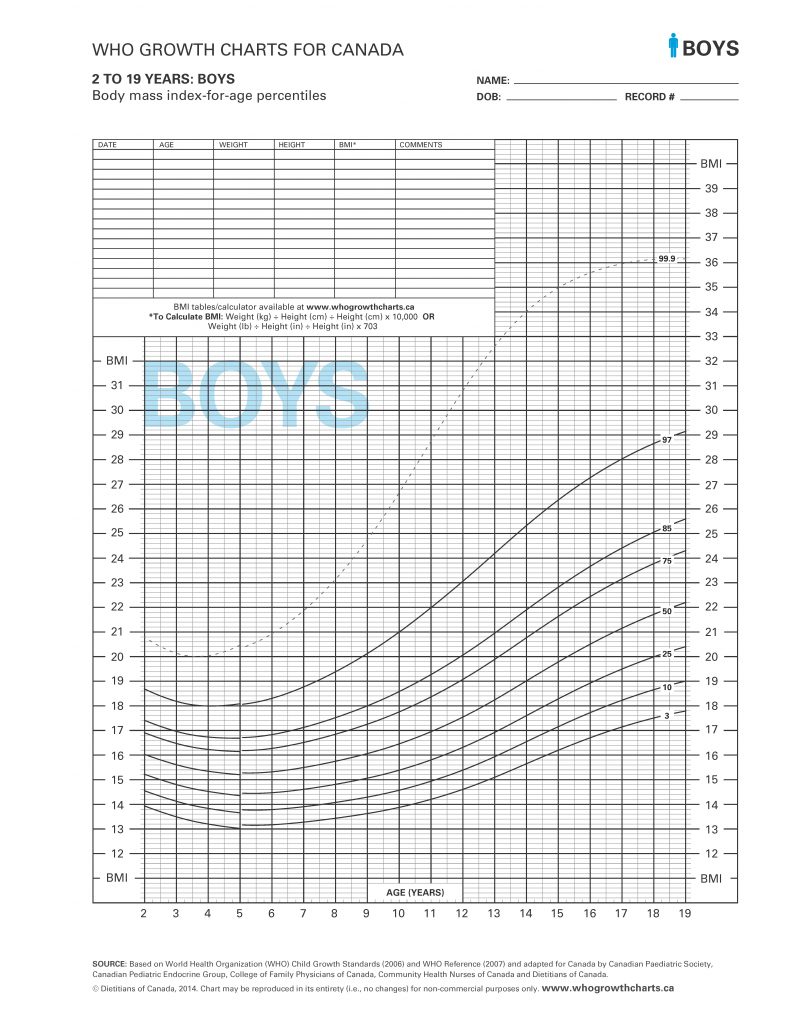
Significant weight gain noted, especially within first three months of medication use and/or child is overweight, obese or has pre-existing metabolic conditions prior to starting SGA treatment
Recommendation:
1.Lifestyle intervention
Second generation antipsychotic medication use in children and youth is associated with weight gain and metabolic complications. It is therefore strongly recommended that patients receive counselling (nutrition, lifestyle and exercise) at the initiation of therapy regardless of baseline body mass index. This is particularly important in a child who is overweight, obese or has existing metabolic symptoms prior to treatment with a second generation antipsychotic medication.
2. Re-evaluate use of SGA to minimize weight gain
Consider the following questions:
2. Fasting plasma glucose and insulin complications management guidelines:
Normal FPG = FPG < 6.1 mmol/L
Recommendation: Repeat FPG check at next scheduled screen. If the fasting insulin is above the upper limit of normal for the assay being used, consider an oral glucose tolerance test (OGTT) and specialist consultation. For those individuals with an FPG value of 5.6 to 6.0 mmol/L, consider an OGTT.
Impaired FPG = 6.1 to 6.9 mmol/L
Recommendation: Consider OGTT and specialist consultation if abnormal. Consider metformin in consultation with a specialist.
Abnormal FPG = FPG ≥ 7 mmol/L
Recommendation: Consult with specialist for the management of diabetes.
Normal weight gain associated with growth and development
Recommendation: Repeat weight measurement at next scheduled screen. Provide information on the importance of lifestyle for decreasing risk of weight gain.
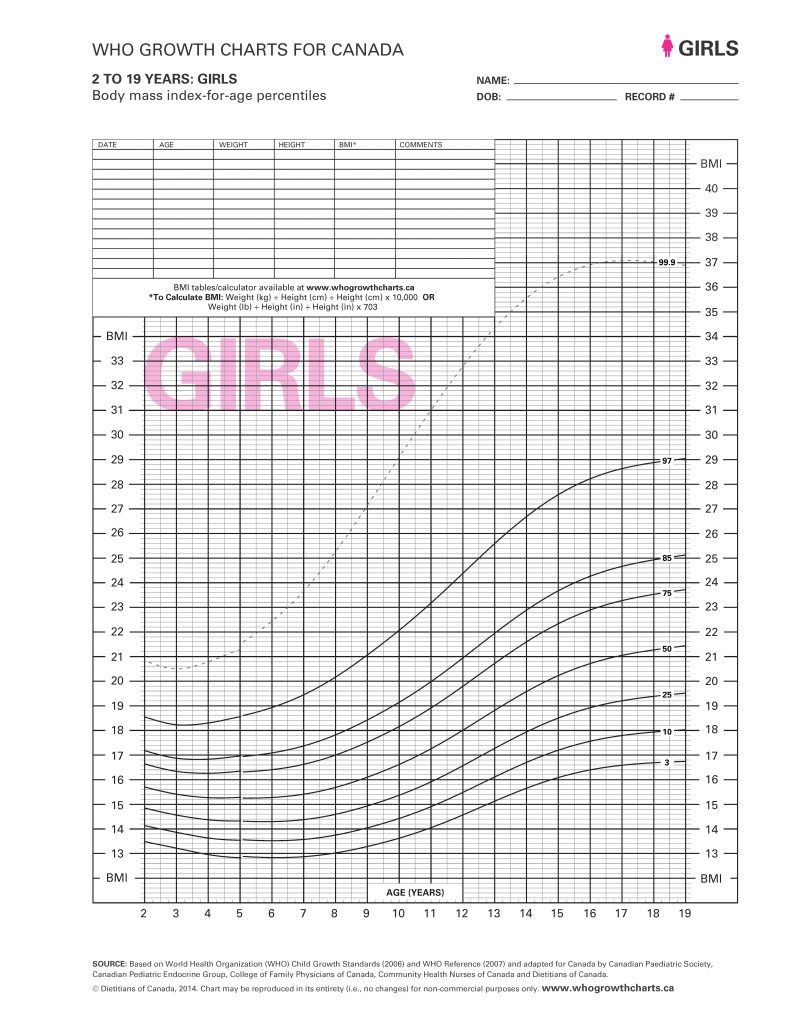
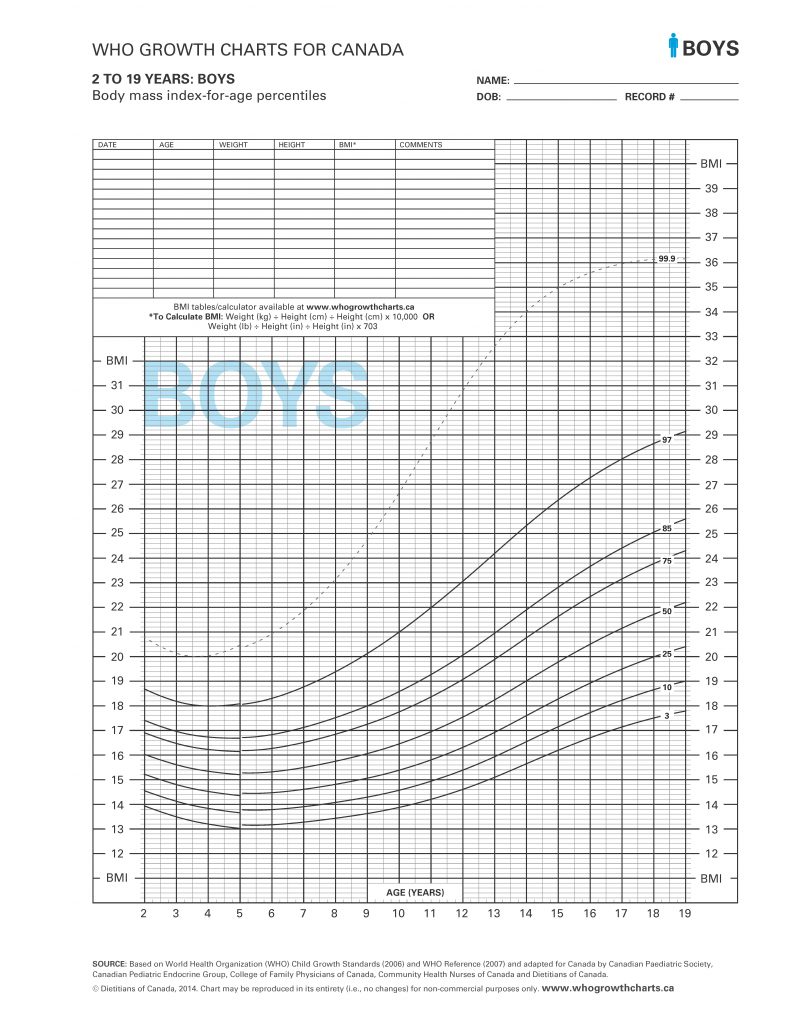
Significant weight gain noted, especially within first three months of medication use and/or child is overweight, obese or has pre-existing metabolic conditions prior to starting SGA treatment
Recommendation:
1.Lifestyle intervention
Second generation antipsychotic medication use in children and youth is associated with weight gain and metabolic complications. It is therefore strongly recommended that patients receive counselling (nutrition, lifestyle and exercise) at the initiation of therapy regardless of baseline body mass index. This is particularly important in a child who is overweight, obese or has existing metabolic symptoms prior to treatment with a second generation antipsychotic medication.
2. Re-evaluate use of SGA to minimize weight gain
Consider the following questions: