Pediatric mental health and substance use courses for healthcare providers
Courses for Healthcare Providers

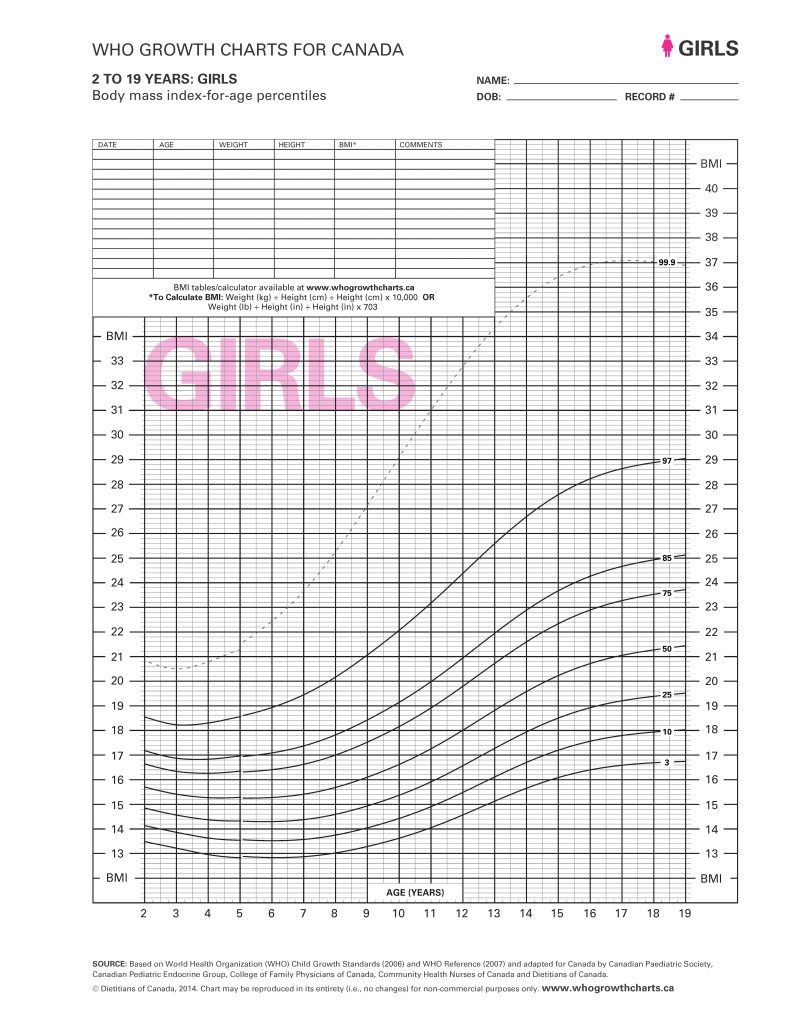
Balanced View
Balanced View is a free evidence-informed online learning resource designed to reduce weight bias and stigma among medical professionals, mental health professionals, allied health professionals and public health professionals.

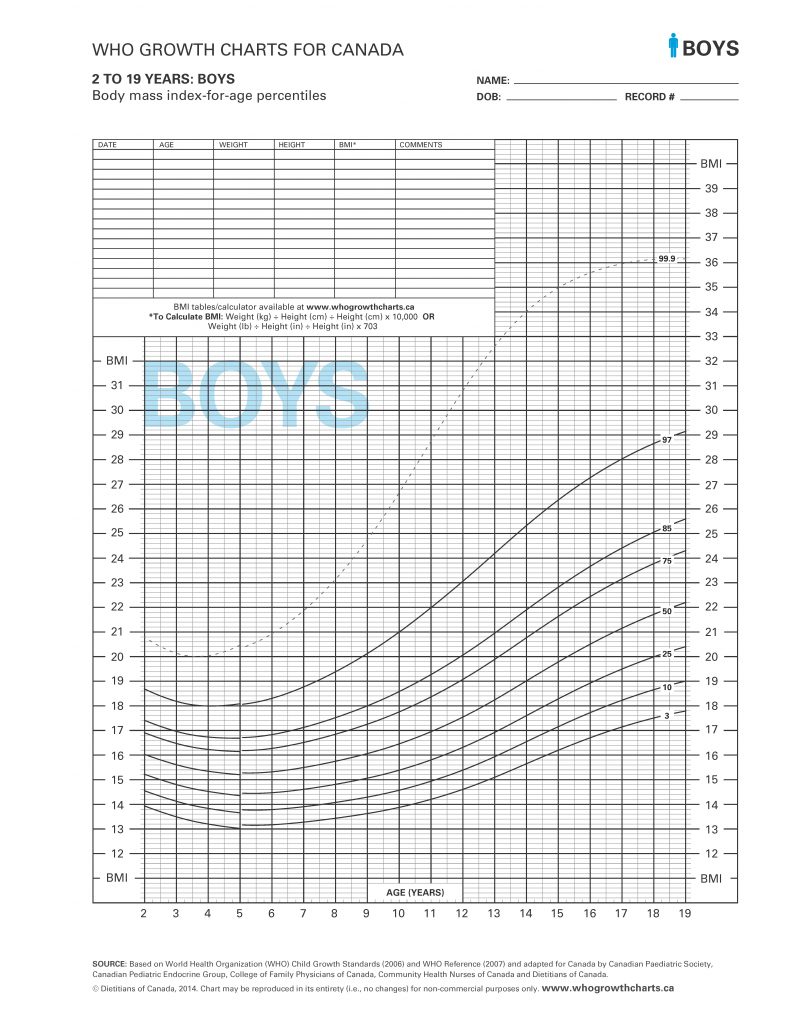
Metabolic Monitoring
Learning Program
An overview of first-generation antipsychotic (FGA) and second-generation antipsychotic (SGA) use in BC and Canada as it relates to children and youth.

Missing Middle
An interactive e-learning program for all health care providers working with youth and young adults who want to deepen their knowledge and skills. Each module features real-life stories, interactive activities, and self-assessments to reinforce learning.
CanREACH
A 3-day interactive course where participants will build skills in assessing, diagnosing, and treating common mental health concerns in children and young people.

Health Promotion
An introductory course about health promotion and disease prevention, and how you can apply health promotion strategies to enhance patient outcomes, strengthen community well-being and advance your work.
CanREACH
A 3-day interactive course where participants will build skills in assessing, diagnosing, and treating common mental health concerns in children and young people.

BC Youth
Mental Health Act

Balanced View
Balanced View is a free evidence-informed online learning resource designed to reduce weight bias and stigma among medical professionals, mental health professionals, allied health professionals and public health professionals.

Missing Middle

Metabolic Monitoring
Learning Program
An overview of first-generation antipsychotic (FGA) and second-generation antipsychotic (SGA) use in BC and Canada as it relates to children and youth.

BC Youth
Mental Health Act
Looking for more resources or clinical support for child, youth, and young adult mental health and substance use?
PHSA provides specialized health care services to communities across British Columbia, on the territories of many distinct First Nations. We are grateful to all the First Nations who have cared for and nurtured the lands and waters around us for all time, including the xʷməθkwəy̓əm (Musqueam), Skwxwú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations on whose unceded and ancestral territory our head office is located.